Touchless Travel: automation in airports post COVID-19
Automation in airports may enable touchless travel. The global COVID-19 pandemic has caused widespread disruption around the world and brought with it a lot of uncertainty. The response from many healthcare systems and technology companies highlights the increased adoption of digital tools and innovative solutions.
Curzon Consulting Partner Chetan Trivedi interviews innovators in the UK healthcare sector. In his latest conversation, Chetan explores automation in airports post COVID-19.
Bob Kwik, Director Europe at Elenium Automation, a passenger experience company focused on improving the journey using automation and technology.
The company is also working with hospitals to roll-out self-service triage solutions. Etihad Airways recently announced that it plans to partner with Elenium Automation to trial new technology which allows self-service devices at airports. The technology will be used to help identify travellers with medical conditions, potentially including the early stages of COVID-19. Etihad will initially trial the monitoring technology at its hub airport in Abu Dhabi in May and June 2020.
Get in touch to discuss how digital strategy and transformation can be applied in your organisation.
Contact us for more information or submit a request for proposal to our healthcare consulting team
Virtual Care: delivering healthcare in the new reality
The global COVID-19 pandemic has caused widespread disruption around the world and brought with it a lot of uncertainty. The response from many healthcare systems is showing the increased adoption of digital tools and innovative solutions.
Whilst Virtual Care services are nothing new, the COVID-19 pandemic has pushed Virtual Care solutions like Telehealth to the top of the healthcare agenda. In order to deal with increased demand for healthcare services, governments around the world have pushed through regulatory changes to allow the widespread use of Virtual Care models. These Virtual Care platforms are an indispensable tool in an environment where health systems try to keep up supply (clinical assessments and triage) with demand (patients).
In a post COVID-19 world, care delivery models around the world will be transformed and there will be widespread adoption of Virtual Care models in virtually every healthcare setting. This is part of a wider digital transformation agenda in healthcare. Care that used to take place exclusively in physical settings (e.g Doctor’s office) can now take place digitally. Every healthcare organisation (payors, hospitals, life sciences, pharma, medical devices etc.) across the entire value chain (prevention, primary care, secondary care, tertiary care, social care, palliative care, etc.) are exploring a variety of virtual care models, many of which are enabled by telehealth technology.
Hospitals are already using Virtual Care to improve accessibility, availability and affordability of care. As demands for healthcare services increase, driven by an aging population requiring more complex care, Virtual Care offers a smart way to leverage finite healthcare resources.
Virtual Care and digital healthcare enable a model of care that is more affordable and integrated into patients’ lives. Consumer behaviour is also shifting. As Dr. Eric Topol describes in his book titled “The Patient Will See You Now”, patients seek to access healthcare on their own terms (time and place).
Hospitals and health systems that take a proactive approach towards Virtual Care will be well-positioned to meet patient demands in the future.

Definitions
Virtual care is comprised of four categories:
Real-time interaction with the most appropriate clinical team to support patient requiring immediate advice. Post virtual triage, a follow face-to-face consultation with the most appropriate clinician team (doctor, nurse, pharmacist, etc.) can take place.
Modern information and communication technologies, data such as bio-signals or medical images can be acquired from the patient and then stored or sent to the specialist when needed. The field of Pathology, Radiology, and Dermatology are those using such services already. For example, with a shortage of Radiologists in certain countries, scans can be read and reported on by specialists remotely. If Artificial Intelligence (AI) is layered on top, certain scans can be read by AI to act as a “second pair of eyes” to human reads.
Uses a range of technological devices in order to remotely monitor clinical signs and health of a patient. Remote monitoring is extensively used in the management of chronic diseases such as asthma, diabetes mellitus, and cardiovascular disease.
According to the Centers for Disease Control and Prevention, 6 in 10 adult Americans live with at least one chronic disease and 4 in 10 adults live with two or more chronic diseases. Among the benefits of virtual care include greater patient satisfaction, more frequent monitoring, and cost effectiveness.
There is a strong tendency that patients are involving more in monitoring their own health through the use of smartphone applications and wearable devices designed to help them track and improve various health indicators.
According to Statista, there are 3.2 billion smart phone users out of a total population of 7.7 billion people around the world. This information and these devices can be also used by policymakers, practitioners, and leaders in the medical and health care industry in order to identify and act on health trends, inform treatment decisions, and even provide outgoing communication to the public.
Such solutions can also deliver basic care to parts of the population living in remote locations. For example, nutrition advice can be provided remotely to pregnant women and/or mothers with young children in small villages with virtually no access to care, but may have access to mobile technology.

“Use” cases
By increasing access points and redistributing expertise where it’s needed, Virtual Care can address disparities and improve outcomes. Virtual Care platforms can be used to provide a range of services such as, but not limited to:
Primary Care
- Chronic care management, recording vital signs through home-monitoring systems and sending alerts to clinicians when readings fall out of the normal range.
- Pharmacy services, including medication review and prescription verification, for patients with chronic diseases such as diabetes, hypertension, etc.
- Diagnostic screening for diabetes-related eye disease, increasing the number of diabetes patients who receive eye exams to help prevent blindness.
- Sleep disorders, monitoring patients with sleep apnoea for sleep patterns, body positions and breathing.
- Tele-psychiatry, assisting patients in need of behavioural health services.
- Tele-physiotherapy, assisting patients with physiotherapy sessions remotely.
Acute/Hyper-Acute
- Tele-stroke services, creating access to the limited supply of stroke neurologists and targeted use of therapies that preserve brain function and save lives. Tele-stroke services can also help facilitate a “hub and spoke” model, where a hyper-acuity stroke unit can provide remote support to a stroke centre.
- Tele-ICU tools, providing 24-hour intensive support to deliver optimal local care to the most acute patients. ICU beds can all be monitored from one, central control room anywhere in the world.
- Pre & Post Op Consultations, ensuring more efficient use of resources across the health system where a physical exam on the day is not required. For example, a patient scheduled for a cardiac ablation procedure can be consulted remotely prior to the procedure, once certain tests have been performed in advance.
- Post-surgical recovery, allowing patients to self-manage recovery process with support from clinical teams as needed remotely. Sophisticated solutions can also include apps to capture progressive pain scores, wound images, etc. so that clinical teams can monitor recovery remotely.
Adoption Challenges
There are some barriers to expanding access to care through Virtual Care. The eight most significant barriers are:
- The lack of leadership and organisational commitment to develop an overarching strategy and integrate care delivery within the clinical pathway (e.g. pre and post op consultation)
- Inadequate clinical engagement and readiness without consideration of user (clinicians and patients) experience and workflows
- Restrictions on how Virtual Care services are reimbursed
- Licensure laws and regulations that limit the ability to provide Virtual Care services across multiple jurisdictions (i.e. from one state to another within the US)
- The lack of “connectivity” or adequate internet services in some areas to support Virtual Care
- Decentralised departmental solutions and pilot programs without governance structure and dedicated management and potentially competing propositions
- The high cost of technologies and infrastructure and a lack of funding
- Evolving measures of success and key performance indicators hampering scaled platforms
As a result of COVID-19, many of these hurdles are being taken down rapidly to help drive quicker adoption of Virtual Care services.
Key Success Factors
How do hospitals and health systems begin to harness the benefits of Virtual Care?
Virtual Care is not about technology. Technology is simply an enabler! It starts with culture—and culture starts with the Board and Executive Management team. The governing board and senior management can ignite cultural change with a vision statement that embraces virtual care as an extension of what the hospital or health system already does, rather than as something new or different.
Successful hospital and health system Virtual Care programs require discerning technology choices and critical vendor selection. Success also demands uncomfortable cultural changes and the right executive to create a comprehensive virtual care delivery system for patients.
We can help your organisation develop a business case for virtual care. We can help you redesign clinical pathways so that virtual care is not a standalone model, but is truly integrated into the delivery of patient care along the entire pathway.
Contact us for more information or submit a request for proposal to our healthcare consulting team
Healthcare change: a perfect storm is brewing
Curzon Consulting Healthcare lead, Chetan Trivedi, argues that a perfect storm is approaching in Healthcare, and it’s been brewing for a while…
On one hand, we are seeing an ageing population, with growing multiple comorbidities, requiring more complex care. On the other hand, according to the International Monetary Fund (IMF), in 2017, global debt had reached an all-time high of $184 trillion in nominal terms, the equivalent of 225 percent of GDP.
In order to “move the needle”, Healthcare systems need to radically move away from “tinkering round the edges”, and instead, focus on delivering transformative change (focusing on prevention, implementing new care delivery models enabled by technology, better triaging and stratifying patients to determine best intervention point (hospital, community, home, etc.), leveraging appropriate skills set to treat patient (physician versus pharmacists versus nurse, etc.).
Some of the choices may not be popular, but if left unchecked, on the current trajectory, we will leave the future generation with a formidable challenge.
So, what are the 10 factors generating the perfect storm in healthcare?
1. Economic headwinds
Unprecedented level of total global debt-to-GDP (225%)* during peace time. Simply printing more money, creating more debt or throwing more funds at an outdated healthcare system is not going to help. Health systems need to improve quality and reduce cost-per-capita quickly. Focus on evidence-based disease prevention is key.
*Global debt has reached an all-time high of $184 trillion in nominal terms, the equivalent of 225 percent of GDP in 2017. On average, the world’s debt now exceeds $86,000 in per capita terms, which is more than 2½ times the average income per-capita. International Monetary Fund, 2019
2. Demographic time-bomb
An aging population with multiple comorbidities is requiring more complex care, so healthcare patients need to be better triaged and stratified to determine the best intervention point (hospital, community, home, etc.). The global population aged >60 years numbered 962 million in 2017, more than twice as large as it was in 1980. This figure is expected to double by 2050.**
3. Disease burden proliferation
We are seeing an increased prevalence of long-term chronic conditions such as hypertension and Type 2 diabetes. These are likely to add pressure on primary and secondary care organisations. Healthcare systems need to radically re-think “healthcare” with a greater focus on prevention and alternative care models such as community, home; GP vs. Pharmacist vs. Nurse.
4. Capacity constraints
The overcrowding of hospitals and emergency departments by patients who can been seen outside of the acute setting are causing delays for patients with higher levels of acuity to be seen earlier. Healthcare patients need to be better educated, triaged and stratified to determine the best intervention point (hospital, community, home, etc.).
5. Regulatory changes
Regulators are increasingly playing catch up with a fast paced, rapidly evolving healthcare sector, particularly with respect to innovation and technology. Commissioners are also pushing for greater cost transparency across the entire healthcare sector (i.e. hospital and drug pricing in the US, diagnostic and drug pricing in India, etc.)
6. Technology disruption
Rapid advancements in Artificial Intelligence (AI), Blockchain, Genomics, Telehealth, Remote Monitoring technologies and customised medicines are allowing clinicians to deliver precision healthcare, whilst improving patient experience and lowering cost. Innovation promises to deliver speed, quality and productivity at scale and lower cost.
7. Patient expectations
Consumer expectations are rapidly rising. Younger patients are increasingly seeking to access care on their terms. The Patient-Doctor relationship is being transformed (“The Patient Will See You Now”***). Older patients are expecting far greater quality of life until much later in life, placing a major strain on healthcare systems such as orthopaedics and physiotherapy.
***The Patient Will See You Now, authored by American cardiologist, geneticist, and digital medicine researcher, Eric Topol
8. Healthcare model transformation
There is increasing pressure to develop high quality, less-expensive alternatives to traditional hospital care models. Increasing focus on delivering care in the community and patient’s home. Move towards Integrated Care, Value Based Outcome, etc. models to drive convenience, improved quality and aligned incentives (payers vs. provider).
9. Challenging treatment protocols
Pressure from patients and clinicians to challenge existing disease treatment protocols. For example, healthcare patients with long term chronic conditions such as type 2 diabetes experimenting with low-carb diets to stop and reverse disease. Focus on prevention through life style changes.
10. Healthcare data explosion
An exponential increase in electronic data is being generated across the Healthcare continuum. AI and connected medical devices will take data generation and storage requirements to a scale not seen before. Securing all this data (on potentially a Blockchain) will be a leading priority for all stakeholders across healthcare.
Sign up to receive future healthcare insights to your inbox.
Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.
Contact us for more information or submit a request for proposal to our healthcare consulting team
Patient experience: the case for home dialysis
We have just completed a major assessment of hospital, satellite and home dialysis delivery models.
Home dialysis: a cost effective solution that improves quality of life
We reviewed the efficacy and cost models associated with hospital, satellite and home dialysis models in multiple countries. In conclusion, whilst it’s not a one size fits all solution, home dialysis is a clear winner for the majority of people on dialysis.
Not only is a home dialysis solution 30-60% more cost effective over hospital and satellite models, it allows patients to perform dialysis in the comfort of their own home, significantly improving quality of life. No longer do patients have to visit a hospital or satellite centre 3 times per week/4-5 hours a session (incl. avg. commute time).
In addition, patients at home can perform nocturnal dialysis, which allows them to maintain a normal working life, which it itself results in wider benefits to the individual and society.
What is Chronic Kidney Disease?
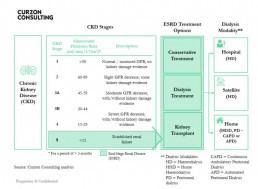
- There are 5 stages of Chronic Kidney Disease (CKD). Stage 5 is classified as end stage renal disease and is when a patient requires renal replacement therapy (transplant or dialysis)
- The Glomerular Filtration Rate (GFR) measures the amount of blood that passes through the tiny filters (glomeruli) in the kidneys, each minute
- The National Service Framework for Renal Services defies normal renal function as estimated GFR = />90 ml/min/1,73M2
- As Chronic Kidney disease (CKD) progresses the GFR falls
- Patients in ESRD have three treatment options:
1) Conservative Treatment – manage symptoms of kidney failure via lifestyle changes
2) Dialysis Treatment – conduct haemodialysis or peritoneal dialysis
3) Kidney Transplant – replace kidney; more cost effective over 10 years than dialysis, but shortage of donors, means dialysis segment will grow - Patients who commence dialysis can have their treatment at a hospital, satellite (standalone clinic) or home
- Haemodialysis and Peritoneal dialysis have similar long-term survival rates
How prevalent is Chronic Kidney Disease in England?
- In England, there are an estimated 2.8m diagnosed and undiagnosed people (6.1%) of the population (>16 years old) that are thought to have CKD (Stage 3-5).
- In 2018, total population in England was ~56m, of which, >16 years old accounted for 45.4m (81%)
- CKD affects ~2.8m people over the age of 16. An estimated ~60,000 patients have End-Stage Renal Disease (ESRD), of which, ~30,000 are on dialysis
- Prevalence rates are rising, largely due to better detection (2.4% in 2007, 4.3% in 2010 and 6.1% in 2017), poor nutrition and lifestyles, which is likely to cause pressure on health budgets
- Prevalence of chronic kidney disease stage 3-5 is expected to increase to 3.2m people by 2021 and 4.2m by 2036
- There are ~40,000 premature deaths every year due to chronic kidney disease (that’s enough people to fill the Royal Albert Hall nine times over)
- Chronic kidney disease diminished quality of life for many people and represents a significant financial burden on the NHS
- Black, Asian and minority ethnic communities are five times more likely to develop chronic kidney disease than other groups
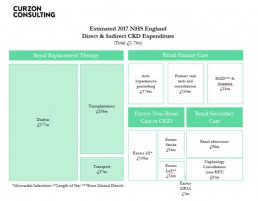
What are the costs of Chronic Kidney Disease in England?
- NHS England spends £1.7bn per annum on CKD (more than the combined £1.4bn cost to treat breast, lung, colon and skin cancer)
- Patients with CKD are likely to develop other health conditions, namely Hypertension, Stroke and/or Myocardial Infarction, resulting in adjacent costs in other non renal areas
- Mean annual direct cost of Dialysis care per patient is estimated to be £577m/30,000 = £19,233
- Full reimbursement by NHS and free at point of care
Source: Public Health England, CKD Prevalence Estimates published in 2014; Chronic Kidney Disease in England – The Human and Financial Cost; Curzon Consulting analysis
Annual dialysis cost by modality (hospital, satellite and home)
Home dialysis solution is not for all patients. Based on our analysis, when home dialysis is utilised, it can cost up to 40-60% lower than dialysis performed in hospitals and 30-40% lower when compared with satellite clinics
The total annual cost of delivering APD and CAPD is substantially lower than that for HD.
Studies in Belgium, Canada, France, Germany, Italy, Japan, Netherlands, Spain, Sweden, Switzerland, UK and USA also found home-based modalities to be more cost effective.
In some countries, two patients can be treated on CAPD versus HD.
Despite overwhelming clinical and commercial evidence, home-based dialysis remains a small segment.
Payment models drive perverse incentives and therefore influence modality selection.
Find out how we can help you to design and implement this solution
If you’d like to learn how to design and implement an evidence-based home dialysis proposition, which can significantly reduce cost and transform patient quality of life, please get in touch.
We can help you to design and implement an evidence-based home dialysis proposition, which can significantly reduce cost and transform patient quality of life.
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.
CONTACT US TO FIND OUT HOW WE CAN HELP
Mobile stroke units - a stroke management study
Curzon Healthcare lead Chetan Trivedi has just completed an extensive study of Mobile Stroke Units (MSUs) in Australia, Argentina, Canada, Germany, Norway and the United States of America.
Our study included a detailed review of the efficacy of stroke management solutions, including the impact on economic and social costs downstream. We have also performed a detailed assessment of people, process and technology required to implement such solutions in other countries. Whilst our example shared below is focused on the UAE, a MSU can be implemented by any health system.
By adopting a Mobile Stroke Unit model, a health system can increase stroke survival rates, reduce disabilities and optimise the associated economic and social cost of care for stroke survivors through drastically decreasing “alarm-to-scan” and “scan-to-treatment” times.
Given our extensive intellectual capital (research and analysis) on the topic, we are able to develop a high-level business case within a few weeks for a local, regional or national health system.
Opportunity to Revolutionise Stroke Management in United Arab Emirates
By adopting a Mobile Stroke Unit (MSU) model, the UAE can increase stroke survival rates, reduce disabilities and optimise the associated economic and social cost of care for stroke survivors through drastically decreasing “alarm-to-scan” and “scan-to-treatment” times.
1. Situation
- There are two key types of stroke: ischemic and haemorrhagic
- Globally, ischemic stroke is the most common, occurring 85% of the time; but whilst haemorrhagic strokes only occur 15% of the time, they are responsible for 40% of deaths
- In the UAE, stroke is the third leading cause of death – “10,000 people suffer from stroke… every year”
- Stroke is the “number one cause of disability” – with only “10% of victims reaching a hospital on time to make a full recovery”
- Stroke “is estimated to cost the UAE around AED 3 billion per year, with additional cost to the economy of a further AED 4 billon in lost productivity, disability and informal care”
- The UAE had no stroke units in 2014 versus 12 in 2019, which is a major step in the right direction
- “The average age of occurrence of stroke is 45 in UAE which is much lower than the world age of 60 years”
Stroke is a major problem for health systems
2. Complication
- 2,000,000 brain cells/ neurons are lost every minute after a stroke, which translates to “Time is Brain”
- The earlier the stroke patient is diagnosed and treated, the better the patient outcomes, leading to a significant reduction in total cost of treating the patient over the life of their associated disabilities
Typical traditional model for stroke treatment is:
- Patient transported via ambulance into Accident & Emergency (A&E) or a specialist stroke unit
- Type of stroke determined by CT scan (a stroke patient cannot be treated until the type of stroke is determined)
- Treatment is administered based on stroke type (ischemic and haemorrhagic)
Through-out the entire process (from acute symptom onset to treatment), significant time is lost, which results in higher mortality risk and additional complications downstream
Correct diagnosis and time to treatment is crucial
3. Question
Despite great progress made in stroke intervention in the UAE in recent times, what can the UAE do to deliver transformative change to increase post stroke survival rates, reduce disabilities associated with stroke, improve patient quality of life post stroke and reduce the associated economic burden on the stroke patient, their family and wider society?
4. Solution
- Instead of patients being transported to A&E or a specialist Stroke Unit, losing valuable time, a specialist Mobile Stroke Unit (MSU) can travel to the patient to deliver emergency point-of-care diagnosis and treatment onsite
- The Mobile Stroke Unit solution was pioneered in Germany back in 2011 and such solutions are being delivered in Australia, Argentina, Canada, Germany, Norway and the US
Key Mobile Stroke Unit attributes typically include:
- appropriately trained emergency response team (e.g. driver, paramedic, critical care nurse and CT technician, optional Vascular Neurologist)
- a Computerized Tomography (CT) scanner
- a point-of-care laboratory system (e.g., serum sodium, potassium, chloride, ionized calcium, total CO2, glucose, etc.)
- a telehealth solution, where a Vascular Neurologist and Pharmacist can video call into the Ambulance to provide guidance to the paramedic team
- an Artificial Intelligence solution to provide on-site diagnosis to rule out stroke-like symptoms (e.g. migraines, seizures, Bells Palsy, inner ear problems etc.), which may not be related to stroke
The most important benefit of the Mobile Stroke Unit is rapid diagnosis of the stroke type and treatment with intravenous tissue plasminogen activator (TPA) can be started more rapidly if appropriate
A randomised controlled trial shows, treatment with Intravenous TPA can be started within an average of 38 minutes when patients are treated in an Mobile Stroke Unit compared with 73 minutes under the existing model
Evidence shows on-site stroke treatment improves patient outcomes
Source:
https://www.stroke.org/understand-stroke/what-is-stroke/hemorrhagic-stroke/; The Epidemiology of Stroke in the Middle East, El-Jha et al 2016; https://www.arabhealthonline.com/magazine/en/latest-issue/2019-show-issue/mechanical-thrombectomy-for-acute-ischaemic-stroke-in-uae.html; The mobile stroke unit and management of acute stroke in rural settings, Shuaib and Terakihi 2018; https://gulfnews.com/uae/health/know-the-signs-of-a-stroke-and-where-to-get-help-1.65494094; Curzon Consulting analysis
CONTACT US TO FIND OUT HOW WE CAN HELP
Chairman's Masterclass: "The Challenge of Longevity"
Event: The Challenge of Longevity27 November 2019, London
Event details
Where: Central London
When: 7pm-10pm, 27 November 2019
What: Dinner, Speech from AIG CEO Adam Winslow and Q&A
About the speaker
On 27 November 2019 we will be joined by Adam Winslow, Interim Chief Executive Officer of AIG’s global Life Insurance business, to discuss the Challenge of Longevity.
American International Group, Inc. (AIG) is a leading global insurance organisation with operations in over 80 countries.
Adam is responsible for AIG’s global life business (US and international). He also is a member of AIG’s Life and Retirement Executive Team.
Adam has served as Executive Director, UK Distribution; COO, EMEA Consumer; CEO, AIG Life Ltd (UK), and CEO, International Life and Retirement in London, before he was named Chairman of the Board of the AIG GBN pooling network in January, 2019.
Previous to working with AIG, he served various roles at Laya Healthcare, Aviva, BGL Group, and Allianz Global Investors.
Who should attend?
The Chairman’s Masterclass Dinner Series is a forum for senior business to discuss topical issues under Chatham House Rules.
Typical attendees include Chief Executive Officers, Chief Financial Officers, Chief Commercial Officers, Chief Strategy and Transformation Officers, Managing Directors and business unit Directors.
Register your interest
Complete this form or email events@curzonconsulting.com to register your interest
Please note that spaces are limited.

This is the latest event in our Chairman’s Masterclass Dinner series, providing UK business leaders with insight for over a decade.
Register your interest to attend this event in London, UK.
Please note that spaces are limited.
Other events
CONTACT US TO FIND OUT HOW WE CAN HELP
Blockchain in healthcare: a use case
Curzon Healthcare lead Chetan Trivedi explores how Blockchain in healthcare will revolutionise the billing and payment process. This will result in the complete disintermediation of a vast administrative layer within the healthcare Provider and Payer (private insurer or public commissioner) organisation.
Consequently, Healthcare Providers and Payers will see a huge benefit through a more streamlined process of handling claims and processing payments. The process will also include various steps like checking patient insurance eligibility and coding claims.
Illustrative smart billing and payment process
The example shown below is based on an insured patient, but the process would be similar for the public sector.
1. Upfront
- Insurer and Provider enter into a Smart Contract on Ethereum blockchain
- The smart contract would be self-executing with the terms of the agreement directly written into code
- The smart contract would exist on a distributed and decentralised blockchain network
- Smart contract would permit trusted transactions and agreements to be carried out between Insurer and Provider without the need for manual intervention (Provider and Insurer), central authority, legal system, or external enforcement mechanism
- Each transaction would be completely traceable, transparent, and irreversible
- Automated invoice and subsequent payment would be triggered (i.e. self-billing) inline with pre-agreed protocols and care pathway (incorporated into the Smart Contract)
- Micropayments are triggered after each care package has been completed
- Penalties are built into the Smart Contract and are assessed automatically if Provider fails to meet quality metrics (e.g. readmission rates, infection rates, revision rates, etc.) or poor outcomes (e.g. PROM, Oxford scores)
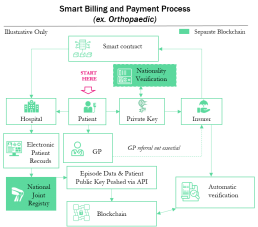

2. Ongoing
- Patient experiences symptoms (e.g. increase pain, reduce mobility etc.)
- Patient visits GP (Physician) or contacts Insurer directly (based on policy guidelines)
- Patient accesses Insurer policy automatically using Private Key
- Insurer automatically routes referral to Orthopaedic Consultant or Provider inline with policy
- Patient commences journey through care pathway (e.g. pre-op, op, post-op, discharge, follow up, etc.) and is treated by the Provider against a pre-agreed set of protocols (consultation, imaging, pathology, implant, physiotherapy, etc.) with the Insurer
- Provider feeds data into Electronic Patient Records (EPR). Standard data linked to specific non identifiable Patient Public Key and is published automatically onto the Blockchain via API
- Insurer automatically validates treatment against pre-agreed care pathway and protocols and automatically triggers payment (see Payment Triggers to left)
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.
CONTACT US TO FIND OUT HOW WE CAN HELP
Increasing patient satisfaction through orthopaedic Enhanced Recovery Programme
The issue
- Reimbursements – Operational and commercial risk transferred from insurer to provider via fixed reimbursements
- Pain – 45%+ patients stated moderate to severe pain within 48 hours of surgery, delaying recovery
- Mobility – Physiotherapy started late usually within 24-48 hours post surgery causing delay in mobility
- Length of stay – 4-6-day length of stay resulting in marginal clinical benefit, unnecessary cost and higher infection risk
What we did
- Established one multidisciplinary team
- Developed Evidence-Based Enhanced Recovery Programme (ERP)
- Established ERP training programme
- Designed and implemented pilot ERP programme (ERP)

The results
- Reduced pain scores by 45%
- Decreased mobility times by 65%
- Shortened hospital stays by 43%
- Reduced hospital cost by 20%
- Increased patient satisfaction by 37%
An award-winning team






CONTACT US TO FIND OUT HOW WE CAN HELP
Reducing 30 day re-admissions by leveraging patient remote monitoring solution
The issue
- Colorectal surgery (related to cancer) accounted for 27% of the total case mix for a large healthcare system
- Colorectal surgery department noticed a steady increase in the number of patients returning back to the Emergency Room (ER) for non-urgent issues over a 24-month period
- 30-day readmission rates were significantly above the national average
- Based on an initial internal assessment, the hospital management and colorectal surgery department hypothesized an issue with the patient discharge process
- Established a cross-functional team to perform a root-cause analysis of the entire patient journey and flow
- Mapped the entire patient journey and flow and identified a number of improvement opportunities
What we did
- Designed a pilot study to test a new discharge process enabled by technology
- Enrolled 97 patients, focusing on younger more tech savvy profile who were open to self-managing recovery during post-operative phase
- Identified root-causes of readmissions into ER (over 78% non-emergency which could have been avoided if patients were better educated and informed during the discharge process)
- Redesigned the discharge programme with a greater focus on patient self-management enabled by smart technology
- Sent patients electronic reminders to help keep them on-track with recovery milestones
- Established post-discharge daily check-ins to track stoma output, incision photos, pain levels, bowel function, etc.
- Implemented algorithms to flag patient issues and automatically provide feedback to patients on how to self-manage or how and where to find relevant support
- Developed intelligent notifications to automatically notify clinical team members if patient at risk
- Designed and implemented a dashboard with real-time reports and analytics to help the care team understand a patient’s post-operative concerns, trajectory of recovery and ways to improve patient experience

The results
- Delivered a 72% reduction in 30-day re-admissions
- Avoided 7 ER visits which were resolved through triage via telephone consultation or outpatient clinic
- Improved patient satisfaction scores by 24% (compared to baseline pre-launch)
- Based on the success of the programme, supported client to identify other surgical programmes to roll-out similar solution
An award-winning team






CONTACT US TO FIND OUT HOW WE CAN HELP
Leveraging procurement to increase profitability of orthopaedic services
The issue
- Many suppliers (18+) resulting in reduced spend leverage
- Prosthesis selection based on supplier systems familiarity not generic technical spec
- Large cost variances for similar hip and knee systems from supplier to supplier
- Large amount of “additional” costs associated with instrumentation and loan kits
- Huge variety in ‘same’ type of hip and knee systems (7+ systems for each)
- Too many system variations (75+) resulting in staff needing to be trained on many systems/brands
- Varying published data to support clinical outcomes of implants resulting in low predictability of patent outcomes
- Huge cost-per-procedure variance impacting profitability at Orthopaedic Consultant and Hospital level
- Need to increase profitability
What we did
- Increased spend with fewer, more capable suppliers
- Established patient profiles. Use patient profiles to guide system selection
Linked into project to Care Pathways - Established minimum acceptance of prosthesis outcomes (leveraging ODEP ratings for both hips and knees)
- Established dedicated training for Orthopaedic Consultants and clinical staff
- Renegotiated with partner suppliers based on redistributed business (volumes)
- Established traffic light reporting for Ortho hip and knee (cost and compliance to agreement)
- Established a clinical advisory group to evaluate innovation and agree protocols to be followed by all Orthopaedic Consultants across the Group

The results
- Delivered 22% in annualised savings through volume leverage and brand/system standardisation
- Reduced clinical risk by only allowing 10 or 10* ODEP rated products and eliminating Orthopaedic work at low volume sites
- Increased profitability substantially which allowed the BD teams to improve NHS and PMI contract win rates
- Reduced supplier power (demonstrated appetite and willingness to shift balance of power)
- Improved patient satisfaction and outcomes by channeling more work to Orthopaedic Consultants with higher PROMs scores
- Reduced subjectivity by ensuring system selection based on patient profile
- Standardised length of stays for given procedure and patient profile
An award-winning team