Hospital-at-Home: an Important Component of an Integrated Care Model
New technology is arming and enabling care providers with the ability to provide seamless support to patients along the entire care continuum. Hospital-at-home care delivery models allow health systems to find the right access and intervention point for delivering targeted patient solutions
The case for change
- Unprecedented levels of total global debt to economic output (debt-to-gdp ratio) during peace time. Simply printing more money, creating more debt or throwing more money at an outdated healthcare system isn’t going to help*
- Aging population with multiple comorbidities are requiring more complex care, so patients needs to be better triaged and stratified to determine best intervention point (hospital, community, home, etc.)
- Increase in prevalence of long term chronic conditions such as hypertension, type 2 diabetes, etc. are better suited to alternative care models (e.g. community, home, etc.)
- Overcrowding of hospitals and emergency departments by patients who can been seen outside of the acute setting are causing delays for patients with higher levels of acuity to be seen earlier
- Rapid advancements in telehealth and patient remote monitoring technologies are allowing clinicians to observe and examine patients remotely, and at scale, allowing care providers to do more with less
- Consumer expectations are rapidly increasing as they demand better care experiences and improvement in quality of life
- Pressure from payers to develop high quality, less-expensive alternatives to hospital care
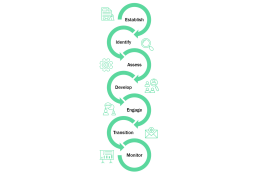
7 key considerations for a Hospital-at-Home Model
- Establish clear objectives of why your organisation is seeking to set up a hospital-at-home model. For example, is it to drive early discharge, optimise admission avoidance, diversify income stream, etc.
- Identify conditions e.g. congestive heart failure, chronic obstructive pulmonary disease, community acquired pneumonia, etc. suitable for home care delivery models based on clinical evidence. Establish patient qualification criteria for hospital-at-home programme.
- Assess patient suitability (against qualification criteria), including functional risk assessment for hospital-at-home care model. Assess patient home for safety / hazards, heating, etc.
- Develop a personalised care plan upon first care provider visit. Personalised patient care plan can be developed by a doctor, pharmacist or nurse (the latter two under the supervision of a doctor using a telehealth solution if needed).
- Engage with patients and caregivers (family members or friends). Ensure anyone supporting the patient at home is part of development of the care plan. Where appropriate, self management (with clinical support) of treatment /condition must be discussed and agreed with patient.
- Prepare patient transition from hospital-at-home programme to primary care setting. Send discharge summaries to the patient’s primary care doctor via electronic patient records system, email, etc. The transition is absolutely key and must be handled flawlessly to avoid patient “falling through cracks”.
- Monitor and provide 24/7 coverage should patient require readmission. Provide in-home diagnostic tests, medications, and equipment (if necessary). Engage with care providers in wider community as needed (e.g. palliative care services, mental health).
*Global debt has reached an all-time high of
About the author

Chetan Trivedi
I lead Healthcare at Curzon Consulting.
For over 15 years I have supported Healthcare payers, providers and medical devices companies on strategy, operational improvement and digital transformation engagements across the UK, wider Europe, Middle East, US, India and Canada.
I am deeply passionate about improving health outcomes, safety and quality of life for patients.


